Start improving with Life QI today
Full access to all Life QI features and a support team excited to help you. Quality improvement has never been easier.

Organisation already using Life QI?
Sign-up
Whilst identifying and proving a changes result in improvement is commendable, the sustainability of the changes is the real measure of long term success! Once your QI project is implemented you may think that your job is done. But what use is an improvement without the conditions to ensure it is maintained? To sustain continuous QI can be a carefully orchestrated balance of conditions, ranging from leadership, to measuring success, to consistency, all of which we are going to explore in this article.
What do we mean by sustainability in the context of QI? In the NHS Institute for Innovation and Improvement's 'Improvement Leaders' Guide to Sustainability and its relationship with spread and adoption,' sustainability is defined as: ‘In its simplest form, sustainability can be seen as ‘holding the gains’ and ‘evolving as required’.’ However, the authors warn that sustainability ‘can also be complex and ambiguous, leading to a variety of perspectives.’
Sustainability in healthcare does not come without its challenges, which can stem from the people within your organisation. Therefore, it's important to meet the conditions before attempting the change, otherwise this can damage the chances of sustaining improvement.
Let’s take a closer look at the challenges, conditions and key factors for sustainability!
There are plenty of changes and innovations implemented in healthcare, but some may not ‘stick’ and could eventually fail. Let’s look at the major challenges for sustaining change.
The NHS Institute for Innovation and Improvement’s guide looks at the challenges for sustainability. The first hindrance the authors identify that is encountered with sustainability is the ‘improvement evaporation effect or initiative decay’. With this, the improvement provided by the innovation disappears over time, and the processes reverts back to how it was before.
Improvement in healthcare requires constant upkeep, as the ‘evaporation’ effect can happen when those implementing become complacent and believe this change would happen automatically. Sustaining change is continuous. Therefore, the team and organisation must provide sufficient training and education to provide new skills and realign the objectives of the wider organisation, to keep alive the enthusiasm and hunger for adopting change.
Another reason for this evaporation is failure to assign responsibility within teams. The change must be championed by all, and everyone must play their part in sustaining this change. However, this comes with its own challenge – a perception of increased workload. In order to sustain the improvement, staff may view the changing systems, processes and/or care pathways as increasing their workload. This could lead to a lack of engagement and compliance.
The second frustration described by the NHS Institute for Innovation and Improvement's guide is ‘isolated improvements or improvement islands’. This describes a scenario where an innovation is implemented in one area or team or department, but it does not spread into the rest of the organisation, as the improvement fails to influence change elsewhere. This highlights that - in order to sustain improvements - consistency throughout the organisation is critical.
Another test for sustainability is challenging opinion within the organisation. Not all improvements are liked, and not everyone wants change. Such improvements can be perceived as change ‘being done to’ the staff, causing resentment and a lack of enthusiasm, this can quickly become the downfall of the innovation.
Perversely, a challenge can be created further down the line by being too good at embedding the improvement. By working so hard on sustaining the change, the improvement can become so embedded into the organisation’s processes, systems, infrastructure and practices, that it can be too difficult to adapt and evolve to changes.
Clearly there are quite a few challenges for sustainability, but it is so important in order to sustain quality improvement. So what are the conditions you need for sustainability to thrive?
Sustainability is achievable and can easily thrive when it has the right conditions. It is therefore important to assess your organisation’s current structures to determine whether it has satisfactory conditions already in place.
The helpful ‘Sustainability Model and Guide’ from the NHS includes a very comprehensive sustainability model. This model groups important factors under three themes: staff, process and organisations. (See figure 1 below.)
The model has 10 elements that play a vital role in sustaining improvement in healthcare. The guide states that one in three improvement initiatives fail to achieve objectives, which can have significant financial and social costs for the healthcare organisation. By using this model, organisations will be able to plan their improvement process effectively and give it the best chance of being able to thrive and be sustained. The tool enables organisations to assess their conditions against the chances of sustaining change.

Figure 1: NHS Sustainability model
As the ‘Guide on spread and sustainability’ from Healthcare Improvement Scotland explains, a diagnostic tool allows teams to ‘assess the sustainability of their improvement projects and identify areas that need to be addressed’. This improves the chances that improvements will be sustained, as it enables teams to make educated changes and enforce measures as required.
Barker et al. wrote a useful article ‘A framework for scaling up health interventions: lessons from large-scale improvement initiatives in Africa’, which emphasises the importance of the organisation being suitably designed for sustainability. They write that sustainability should be built into each layer of the organisation, from processes and systems, to structure and ongoing education, this is to ensure that the organisation cannot revert to operations prior to the innovation. Along with this, they write that a crucial condition is ongoing leadership. Commitment from leadership helps to replenish enthusiasm when it dips among staff and will sustain continuous quality improvement within the organisation.
Now we know what conditions you need to sustain improvements, what are the key factors in sustainability?
The helpful guide from the NHS Institute for Innovation and Improvement shares that the key factors in sustainability are also the factors for effective spread. For more information on spread please take a look at Article 4 from this series on our website. The guide suggests that there are specific elements that exist within organisations that support changes. Each of these factors are connected to support sustainability and are underpinned by engagement and clinical leadership.
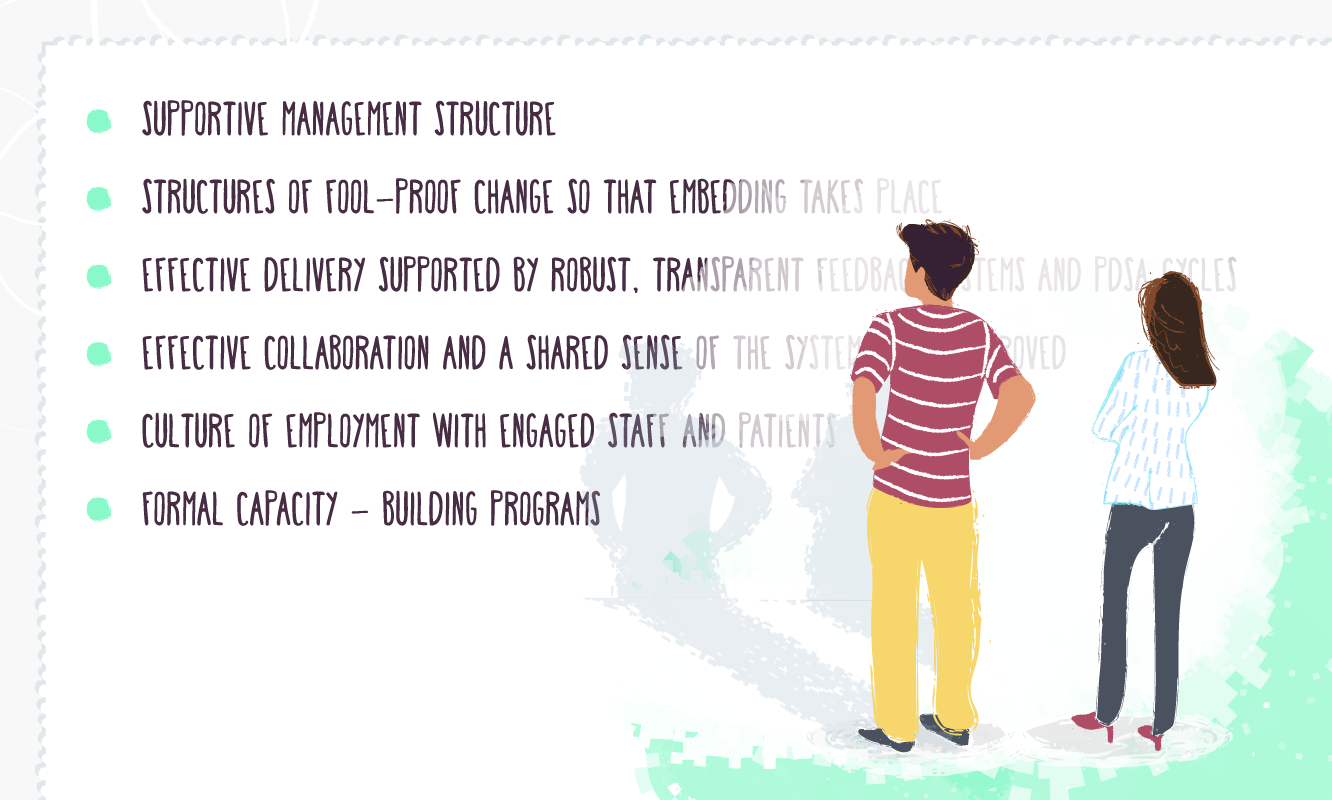
Key factors to promote sustainability are:
Leadership teams can encourage change through championing improvement work, tracking performance, delegating responsibility and celebrating service improvements.
This is to ensure that the organisation cannot revert to old processes. This will mean bringing about organisational changes to policies and practices to make the improvements the new normal. This will ensure embedding takes place.
The organisation as a whole should understand the changes and value its benefits. Alongside this, the organisation must have a measurement system in place, that will review performance and provide data.
Everyone involved should be aware of the processes and systems that the innovation will improve. All staff understand their responsibilities and contribution in the improvement process. This is shared on a diagram mapping out the improvement process, to be shared and analysed between all stakeholders.
It is important to foster a culture of improvement and engagement, colleagues will therefore share a sense of pride and enjoy the improvement process. This helps with diffusing these improvements, as peers will encourage each other to support the innovation.
Ongoing training of staff in clinical and non-clinical disciplines, and the training in the application of modern QI methods. This builds into creating a culture where QI is the norm and integrated into daily processes.
All of these factors supported by engagement and clinical leadership, are essential in order to sustain change and improvement in healthcare.
Along with the above, NHS Education for Scotland succinctly categorised the factors into helpful requirements. Organisations must create a new range of practices adapted to the improvement to make it sustainable. The organisations must have a focus on:
These are the broad categories that must be accounted for when making a change. With these satisfied the organisation will find it very difficult to resort to the old way, this will help to make the new way easy, and the old way harder.
It might seem that sustaining improvement in healthcare isn’t an easy task. However, there are plenty of tools and guidance that an organisation should follow – such as making full use of the NHS diagnostic tool before attempting change. This way many of the challenges will be mitigated from the outset. Along with the conditions, the key factors of sustainability are succinctly stated as, standardisation, documentation, measurement and training. With these requirements implemented, any improvement can be made sustainable.
To finish with the words of NHS Improvement about how successful sustainability should look: ‘New ways of working and improved outcomes become the norm. Not only have the process and outcome changed, but also the thinking and attitudes behind them are fundamentally altered and the systems surrounding them are transformed in support. As a result, when one looks at the process or outcome on year from now or longer, one concludes at minimum that it has not reverted to the old way or old level of performance’.
We hope that this article has shone a light on the steps, the ‘what to dos’, the ‘what not to dos’, to sustain great innovations in your organisation!
Full access to all Life QI features and a support team excited to help you. Quality improvement has never been easier.

Organisation already using Life QI?
Sign-up